Understanding the nuances between C-PTSD, PTSD, and Trauma
As a mental health professional and the owner of Mountain Valley Counseling, I often encounter individuals who struggle with the effects of trauma in various forms. Two terms that frequently arise in my practice are Post-Traumatic Stress Disorder (PTSD) and Complex Post-Traumatic Stress Disorder (C-PTSD). While both conditions stem from experiences of trauma, they manifest differently and can lead to various emotional and relational difficulties, including anxiety and depression. Understanding these differences and similarities is crucial for effective treatment and healing.
PTSD is typically caused by a single, traumatic event, while C-PTSD is usually caused by long-term or repeated trauma. C-PTSD can develop from childhood trauma, such as abuse, neglect, or witnessing a kidnapping. It can also be caused by other types of trauma, such as living through war, being a prisoner of war, or experiencing chronic intimate partner violence.
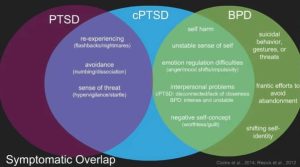
Often people with Cluster B personality disorders, especially Borderline Personality Disorder (BPD)have many overlapping symptoms of C-PTSD. It can take a skilled and specialized therapist to parse out the difference, but it is kind of a chicken or egg scenario. It is very common for people with BPD to also have C-PTSD. Though not every person with C-PTSD has BPD.
Defining PTSD in more detail
PTSD is a mental health condition that can develop after a single traumatic event. The symptoms typically fall into four categories:
- Intrusive Memories: Individuals may experience flashbacks, nightmares, or distressing thoughts related to the trauma.
- Avoidance: Many people with PTSD will avoid reminders of the trauma, including places, people, or activities that trigger memories.
- Negative Changes in Mood and Cognition: This can manifest as persistent negative beliefs about oneself or others, feelings of detachment, and difficulty experiencing positive emotions.
- Arousal and Reactivity: Symptoms may include heightened startle responses, irritability, difficulty sleeping, and difficulty concentrating.
Individuals with PTSD often find that their symptoms arise in response to specific triggers, making their experiences somewhat easier to identify and address in a therapeutic setting.
Defining C-PTSD: Complex Post-Traumatic Stress Disorder in more detail
C-PTSD, on the other hand, is often a result of prolonged or repeated trauma, especially during critical developmental periods such as childhood. The symptoms of C-PTSD overlap with those of PTSD but can be more complex and pervasive. Key symptoms include:
- Emotional Regulation Difficulties: Individuals may struggle with managing their emotions, experiencing intense feelings of sadness, despair, hostility, anger, or anxiety.
- Consciousness and Memory Problems: These might include dissociation, gaps in memory related to the trauma, or difficulty recalling specific events.
- Negative Self-Perception: A common feature of C-PTSD is a pervasive sense of worthlessness or a feeling of being permanently damaged. Can have issues with identify or sense of self.
- Relationship Challenges: Many with C-PTSD have difficulties in relationships, often struggling with trust, intimacy, or feelings of abandonment. Can withdrawal socially and have trust issues. Shame can also come up in the context of relationships.
- Dissociation: Some individuals may experience detachment from their emotions or surroundings, leading to a sense of unreality.
Similarities Between PTSD and C-PTSD
Despite their differences, PTSD and C-PTSD share some common ground. Both are responses to trauma and can cause significant emotional distress. Symptoms of anxiety and depression often accompany both conditions, as individuals may feel overwhelmed, helpless, or hopeless. Additionally, individuals with either PTSD or C-PTSD may experience difficulties in their personal relationships, as trauma can affect one’s ability to connect with others.
Differences in Diagnosis and Treatment
The diagnosis of PTSD and C-PTSD requires thorough assessment by a qualified mental health professional. While both conditions fall under the umbrella of trauma-related disorders, the treatment approaches may differ.
- PTSD Treatment: Traditional PTSD treatment often includes cognitive-behavioral therapy (CBT), which helps individuals process the trauma and develop coping strategies for managing symptoms. Eye Movement Desensitization and Reprocessing (EMDR) is another effective treatment that focuses on processing traumatic memories.
- C-PTSD Treatment: Treatment for C-PTSD may require a more nuanced approach, given the complexities of the symptoms. In addition to traditional therapies, individuals may benefit from therapies that focus on building emotional regulation skills, enhancing self-compassion, and developing healthy relationships. Dialectical Behavior Therapy (DBT) and trauma-focused therapies can be particularly effective for those with C-PTSD. EMDR, Transference Focused therapy, IFS, psychodynamic therapies, attachment based therapies can all be efficacious.
Trauma’s Broader Impact: Anxiety, Depression, and Relationships
Both PTSD and C-PTSD can lead to symptoms of anxiety and depression and issues in relationships. I often see people come to therapy with these diagnoses, which are accurate, but don’t tell the whole picture. These are usually symptoms caused by deeper difficulties and for the purposes of this discussion, symptoms of either PTSD or C-PTSD.
At Mountain Valley Counseling, we emphasize a holistic approach to mental health, recognizing that healing from trauma is a multifaceted process. By addressing the root causes of trauma and developing coping strategies, individuals can work toward reclaiming their lives and fostering healthier relationships. Remember, you are not alone on this journey, and there is hope for healing and recovery.
There is a great new book out called What My Bones Know: A Memoir of Healing from Stephanie Foo that is excellent and explains in great detail what C-PTSD is. Check it out.